Notes on the CTD / Vasculitis pathway for GPs
The connective tissue diseases and vasculitides are heterogenous conditions and can have a wide range of presentations, from insidious to fulminant organ and even life-threatening disease.
If you suspect a patient has a new presentation of vasculitis or organ threatening CTD, please refer urgently to rheumatology during office hours, or general medicine via the admissions suite or Accident and Emergency with plan for rheumatology referral.
There is a rheumatology specialist trainee on call from 9:00am to 7:00pm weekdays and 9:00am to 1:00pm weekends who can give telephone advice and coordinate an urgent admission or urgent out-patient review.
Contact via Switchboard
Telephone: 0191 233 6161
All patients with newly diagnosed ANCA associated vasculitis should be considered as having a potentially severe life or organ threatening disease and therefore should be assessed by a specialist physician with expertise in vasculitis for urgent treatment.
Referrals to the CTD / vasculitis specialist service come from a variety of sources:
- GPs
- in hospital referrals from a range of other specialties
- tertiary referrals from other rheumatology departments, or
- more rarely, community physiotherapists including Connect.
A CTD or vasculitis can be challenging to identify. LUPUS UK has reported that the average length of time their members have had symptoms prior to diagnosis is 7 years. The Behçet’s Syndrome Society found that the average delay for diagnosis for Behçet’s disease is 12 years.
As a department, we are very happy to accept referrals or discuss the indication/appropriateness of referral to secondary/tertiary care. This can be done via Advice and Guidance.
Please refer to Recommendations – Choosing Wisely UK – British Society of Rheumatology (especially recommendations 1 and 6) to decide if you should check autoantibodies.
Please only check in patients you suspect may have a connective tissue disease or vasculitis, avoid in the investigation of widespread pain or fatigue alone.
Auto antibodies are NOT diagnostic tests and should not be used to screen for conditions.
Auto antibodies do not need to be checked before referral to rheumatology.
Helpful websites
Conditions | Types of arthritis, causes, treatments (versusarthritis.org)
LUPUS UK – The National Charity for People Affected by Lupus
The UK’s Leading Vasculitis Charity | Vasculitis UK
SRUK – Scleroderma & Raynaud’s UK | SRUK
British Sjögren’s Syndrome Association, BSSA Charity | Sjogren’s | Sjogrens | Showgruns | Showgrens
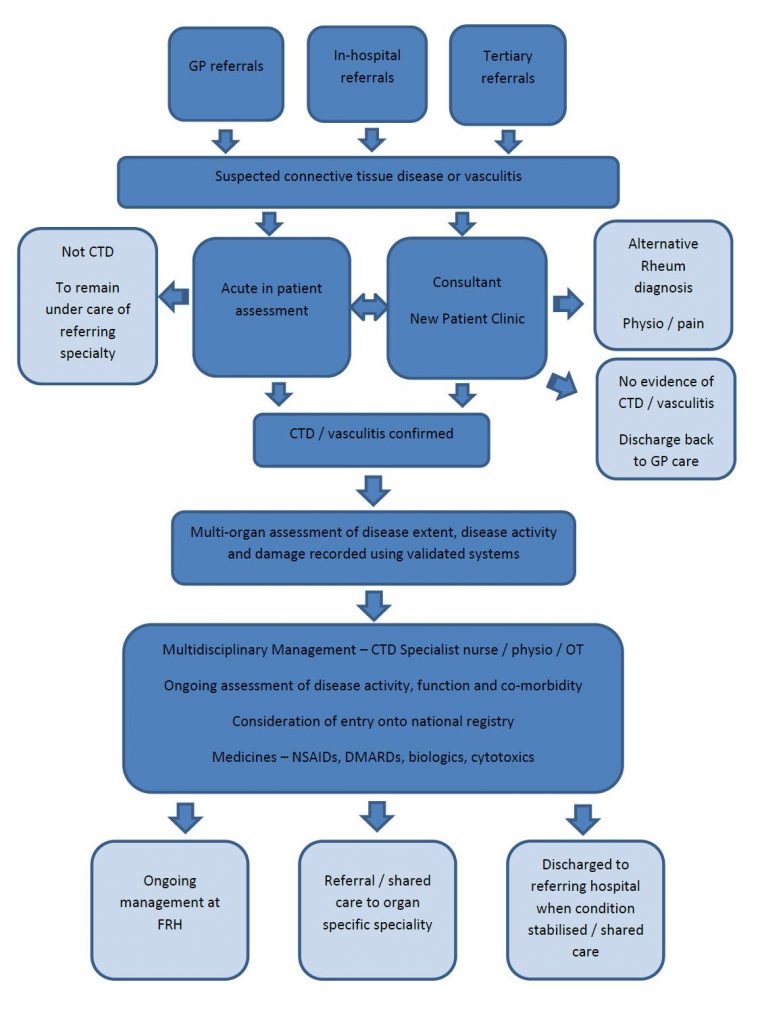
CTD / Vasculitis pathway for GPs
Suspected connective tissue disease (CTD) or Vasculitis
- GP referrals
- In-hospital referrals
- Tertiary referrals
(i) Acute inpatient assessment
- Not CTD – to remain under care of referring specialty
- CTD confirmed – see below
(ii) Consultant – New patient clinic
- No evidence of CTD / vasculitis? Discharge back to GP care
- Alternative rheumatology diagnosis – Physio – pain
CTD / vasculitis confirmed
- Multi-organ assessment of disease extent, disease activity and damage recorded using validated systems
- Multidisciplinary Management – CTD Specialist nurse / physio / OT
- Ongoing assessment of disease activity, function and co-morbidity
- Consideration of entry onto national registry
- Medicines – NSAIDs, DMARDs, biologics, cytotoxics
(i) Ongoing management at Freeman Hospital
(ii) Referral / shared care to organ specific specialty
(iii) Discharged to referring hospital when condition stabilised / shared care
GP Pathway Flowchart for Connective Tissue Disease