The Newcastle Renal Unit was set up under the leadership of Professor Sir George Smart, Professor of Medicine on Ward 9 at the Royal Victoria Infirmary (RVI) in 1957.
Dr John Anderson was the first doctor responsible for day to day running until 1959, when he was appointed Professor of Medicine at Kings College Hospital in London. His successor was Dr David Kerr initially as First Assistant and later Professor of Renal Medicine.
At first dialysis could only be offered to cover kidney failure lasting 2 to 6 weeks until the kidneys recovered as in acute renal failure. If it became clear that the kidneys would not recover, that is the kidney failure was chronic, nothing more could be done.
In 1963 the first kidney transplant was done in Newcastle by Professor John Swinney, Consultant Urologist, and at the same time long term dialysis for patients with chronic renal failure was started.
At first, the dialysis was performed in the basement of the RVI using a twin coil dialyser. A junior doctor (senior house officer) sat with the patient throughout a 12-hour session of dialysis. It was only as the numbers of patients on long-term dialysis increased to around 20 that highly trained nurses took over the task.
As the numbers on dialysis grew, a further small dialysis unit was opened in an old urology operating theatre at Newcastle General Hospital (NGH) and a training program for home haemodialysis was established at the RVI. In addition, long-term treatment by peritoneal dialysis in hospital on 2 days each week was established at NGH.
The Ear Nose and Throat Hospital at Rye Hill in the west end of Newcastle was developed as a hospital haemodialysis unit in 1966 and steadily grew in capacity by introducing 2 daytime and one night shift with each patient initally dialysed twice and later 3 times weekly.
The ever-increasing demand for long-term dialysis was solved by continuing to gradually expand hospital haemodialysis in Newcastle but also by the establishment of independent renal units at Middlesbrough in 1969 and Sunderland in 1970. In addition, with the introduction of the soft silastic abdominal cannulae, peritoneal dialysis at home became possible. Patient training began in 1972 and the numbers on peritoneal dialysis treatment expanded rapidly.
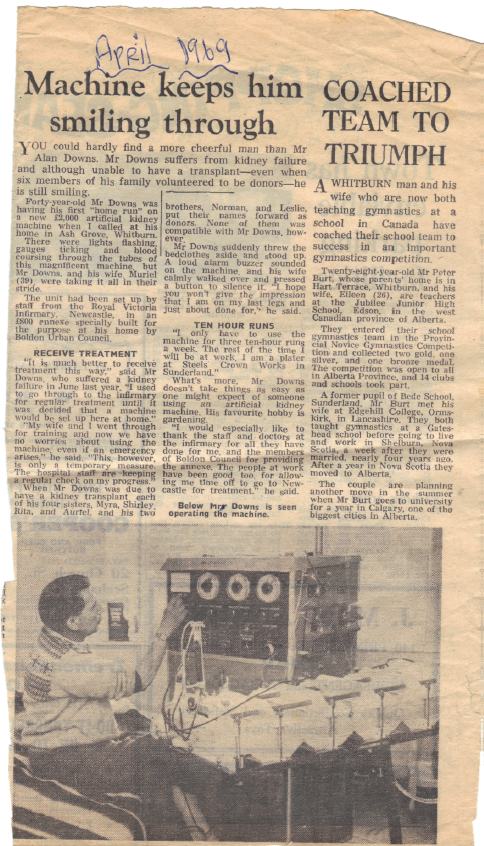
There were also a few patients doing home haemodialysis – here is a local newspaper article from 1969:
The haemodialysis unit at Rye Hill moved to a purpose built dialysis unit at Freeman Hospital in 1979 and a new inpatient renal ward shared the renal service with unit at the RVI.
Following Newcastle’s first kidney transplant in 1963 at NGH, the programme continued under the direction of Professor Swinney and moved to ward 9 RVI in 1966 with expansion of cubical space.
It later moved to the new renal ward in the Leazes wing of the RVI and in 1993 to the renal unit on ward 4 at Freeman Hospital when transplant services for kidney, pancreas and liver were unified to facilitate surgical cover.
Previous staff members
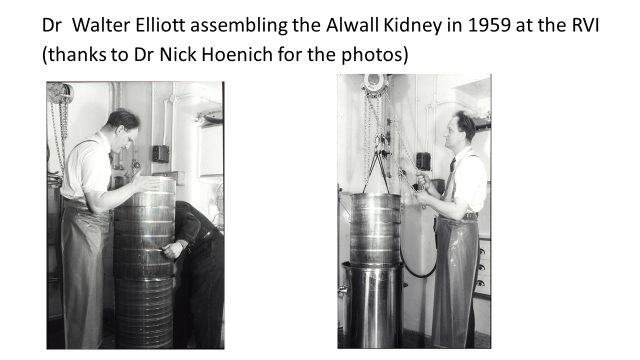
Dr Walter Elliot
Professor David Kerr led a team which included Dr Walter Elliot, who started his medical career training in surgery under Professor John Swinney, Professor of Urology at Newcastle but moved over to the new specialty of Renal Medicine in 1958.
Dr Elliot was one of the pioneers of dialysis treatment and remained a pillar of strength in the renal unit until his retirement in 1994. He was an associate specialist initially and became a consultant nephrologist in 1978. He worked initially at the RVI then moved to NGH and to Freeman Hospital when it opened. He was predominantly a clinical nephrologist but made many research contributions, including the first description of bladder cancer occurring as a complication of treatment with cyclophosphamide.
Dr Robert Wilkinson
Dr Robert Wilkinson joined the renal team as one of the two first senior house officers in renal medicine in Newcastle in 1964. After 5 years of training in general medicine and nephrology at the RVI and 2 years research at Stanford University in California, he returned to the renal unit as Lecturer in Medicine in 1971 and was appointed consultant physician in 1972 and Professor of Renal Medicine in 1989. His main research interest was in the inter-relationship of kidney disease and hypertension and he made important contributions to the understanding of this. He initially worked with Professor Kerr at the RVI but took responsibility for the new renal unit at Freeman when it opened in 1979.
Professor Bob Wilkinson was an outstanding clinician, whose patients were so devoted to him that they would happily wait as long as necessary to be seen by him in clinic, rather than be seen sooner by anybody else. He was able to supervise a research programme whilst carrying out a very heavy clinical workload. Professor Wilkinson was exceptionally supportive to his junior staff, many of whom were inspired by him to pursue a career in nephrology.
Dr Robert Uldal
Dr Robert Uldall joined the renal unit in 1966 after army service and after a period of research into methods of preservation of cadaver kidneys for transplantation he was appointed Consultant Nephrologist in 1969 at NGH. He played a major role in preparing patients for renal transplantation and supervising post-operative care. He did this almost single handed until 1972 when he was joined by Robert Wilkinson in supervising the care of the renal transplant patients. He emigrated to Toronto in 1979 where he continued to make major contributions to the development of dialysis and transplantation.
Mr Ross Taylor
Mr Ross Taylor trained in general and vascular surgery at the RVI under the direction of Ivan Johnson, Professor of Surgery. As a senior registrar he assisted Professor Swinney at the first renal transplant performed at the RVI in 1967 when transplant services moved from NGH. He was appointed Consultant and Senior Lecturer in Transplant and Vascular Surgery in 1970 and became Consultant in charge of renal transplantation when Prof Swinney retired in 1973. He continued in this role until he retired in 1993. As well as directing the surgical transplant team, he led a research group which made important contributions to our knowledge of transplant immunology.
Dr Michael Ward
Dr Michael Ward had his first contact with the renal unit as a medical student when he undertook a research project under the direction of Professor Kerr. After postgraduate training in general medicine and nephrology at Newcastle and the Hammersmith Hospital he was appointed Consultant Physician and Nephrologist in Newcastle in 1980. His main research interest was in the complications of long-term dialysis and he made important contributions to our understanding of renal bone disease. He retired in 2008.
Professor Tim Goodship
Professor Tim Goodship was appointed Senior Lecturer in 1990 having first joined the Renal Unit as a Registrar in 1981. After a period of research examining nutrition in patients undergoing treatment with peritoneal dialysis, he moved to Boston, USA where he undertook further nutritional studies at the Massachusetts Institute of Technology and Harvard Medical School. After his appointment he established a research programme initially in nutrition but later also in renal genetics examining particularly rare renal diseases such as vesico-ureteric reflux (VUR) and atypical haemolytic uraemic syndrome (aHUS).
In recent years he established and oversaw the national service for aHUS including treatment with the complement inhibitor eculizumab. In 2016, the National Renal Complement Therapeutics Centre opened at the RVI, providing national advice on the management of atypical haemolytic uraemic syndrome and C3 glomerulopathy.
Dr John Tapson
Dr John Tapson also joined the renal unit as a senior registrar and was appointed a consultant in 1990. He trained in Guy’s Hospital, London and Brighton, and spent a year in Toronto gaining expertise in peritoneal dialysis, which he brought back to the Newcastle unit. Dr Tapson oversaw the merging of the renal units at the RVI and Freeman Hospital into a single haemodialysis unit on ward 22, and a single renal ward 4 with the renal transplant ward 6a at Freeman Hospital in 1993.
Dr Tapson as renal Clinical Director then worked to develop a new renal ward (ward 32) and dialysis unit (ward 31) within the new NCCC block at Freeman Hospital, which opened in 2009. He also worked with colleagues, notably Professor Derek Manas, to develop the UK’s first dedicated Institute of Transplantation at Freeman, which opened in 2011.
Dr Tapson was a dedicated and outstanding clinician, with a prodigious work rate! He retired in 2014.
Dr Charlie Tomson
Dr Charlie Tomson trained in Oxford and worked in Newcastle as a registrar. He was a consultant in Bristol for most of his career, where he was a key contributor to the UK Renal Association and the UK Renal Registry. He led on many national quality improvement projects, and published widely. He was passionate about patient empowerment and shared decision making.
He moved from Bristol to Newcastle in 2014, and retired in 2019, returning to help with the clinical service during the COVID pandemic in 2020.
Dr Alison Brown
Dr Alison Brown was appointed as the unit’s first female consultant in 1995. Dr Brown trained in Cambridge, and was an SHO on the Newcastle renal unit before further training in Addenbrooke’s and Papworth hospitals, then Bart’s Hospital, London, before returning to Newcastle as a senior registrar.
Dr Brown took over as lead clinician after Dr Tapson’s retirement, and worked with Pam to set up the first satellite dialysis unit in Alnwick. She was Training Programme Director and teaching lead for many years, and introduced Sim training for central lines and renal biopsies – she remains particularly proud of her home-made renal biopsy simulator (a pig’s kidney suspended in raspberry jelly).
The Royal College of Physicians of Edinburgh awarded Dr Brown the RCPE Chiron medal in 2016, in recognition of her excellence in teaching and training.
Together with Professor Talbot, she set up the ISN-TTS sister centre partnership with the transplant unit in Kathmandu, Nepal. She will retire at the end of 2021.
Pam Yanez OBE
Pam Yanez OBE first joined the Renal Unit, Ward 9 at the RVI, in 1974 as a first year Student Nurse and left it in 2014 some 40 years later! Here is her renal journey in her own words:
“As a student nurse I was fascinated by the complexity of the patient care, technical aspects of dialysis and the team approach of working. After qualifying in 1977 I did 15 months as a Staff Nurse in acute medicine to broaden my experience, before undertaking the Renal Course, after which I returned to Ward 9. I became the Junior, then later Senior, Sister on Ward 22 Haemodialysis at Freeman Hospital in late 1979.
“During my time in dialysis I saw many developments. Dialysis equipment changed from a 200 litre Kolff tank to a sophisticated single pass machine. Artificial kidneys from coils to Kiil boards, flat plates to hollow fibre dialysers. Vascular access from shunts to fistulae, grafts to early permanent necklines. Dialysis solution improved from acetate to bicarbonate buffer. Peritoneal dialysis developed from weekly “stab” PD to long term CAPD and APD. This was a time of great progress in dialysis. Later came EPO. The debilitating anaemia became a thing of the past. I took many patients on holiday undertaking dialysis in a variety of places. We all had great fun. My frustration was the lack of opportunity for the patients to have a transplant.
In 1985 I was appointed as the first Transplant Coordinator in the Northern Region. My task was to increase organ donation primarily for the kidney programme but as heart, lung and liver transplantation was becoming established all donors were considered as multi-organ donors. From being single-handed, over a period of time I became the Lead of a team of four. We consistently had the highest donation rates in the UK, giving our patients in the north-east the best chance of having a transplant. Our care of the organ donor families was the most comprehensive in the UK based upon a research project I had undertaken. We held our first Service of Remembrance for our donor families in 1988. The success of our donation programme was due to the wonderful support from our regional Critical Care units and the Emergency Department in Newcastle. Donation from non-heart beating donors (now known as DCD) had been part of our programme for several years. In 1994 we set up our programme, only the second in the UK, in the Emergency Department at the RVI. Our assessment of the suitability of these kidneys for transplantation was based on a visit three of made to Maastricht in order to observe their ground breaking work. Live kidney donation also increased and we were delighted to be part of the assessment process for the donor. In 2002 I was proud to be awarded an OBE for services to healthcare for my work in organ transplantation.
I was appointed as the Directorate Manager (formerly Specialty Manager) for Urology and Renal Services in 2001. I was involved with the planning of the Renal Services Centre and the Institute of Transplantation. Improving the quality of services for the patients was my challenge. I am proud to have been a part of a skilled multi-disciplinary team. My final achievement was securing the agreement of the Trust, after a long and difficult process, to procure a satellite dialysis unit to provide care closer to home.
Throughout my career I have seen so many developments in care of the renal patient. Dialysis has become an option for all instead of a few with the cutting edge technology of today. Transplantation an everyday occurrence instead of a headline in the Evening Chronicle.
We care for renal patient throughout their life from the point of diagnosis. We are a family. I have known some patients for more than 30 years. I remain in awe of their fortitude. The donor families who were so generous at the most difficult time are my heroes. Finally I am proud to have worked with so many dedicated colleagues. I could not omit to mention my “special ones” – Prof David Kerr, Mr Ross Taylor and Prof David Talbot”.