The Posture and Movement Service offers an additional opinion regarding assessment, diagnosis, prognosis and management of children with postural, gait or movement disorders of neurological origin.
Who do we see?
This service is designed to benefit children with movement disorders where there are specific questions regarding diagnosis, prognosis and motor management. There is a particular emphasis on the management of spasticity and dystonia.
Referrals
Referrals may be initiated by any member of the local team, but must be discussed and agreed with the child’s consultant paediatrician or orthopaedic surgeon
Referrals should be directed to Dr Anita Devlin Consultant Paediatric Neurologist or Dr Yasmin DeAlwis Consultant in Paediatric Neurodisability.
A summary of the medical history, together with relevant reports and investigations, should be included. Contact details for the local physiotherapist/occupational therapist are mandatory to facilitate pre-clinic liaison.
The child’s physiotherapist/occupational therapist is welcome to attend the clinic appointment with the family’s permission. Parents are asked where possible to bring to the clinic their child’s usual walking aids and current orthotics/splints.
Team
The posture and movement team is supported by consultant paediatric neurologists, a consultant paediatrician in neurodisability, consultants in paediatric orthopaedics, clinical specialist physiotherapists and occupational therapists, and a specialist registrar.
Clinics
Depending on your child’s needs you will be invited to attend one or more of the following clinics. During your appointment we may ask to video your child.
Research
GNCH is a research active hospital and posture and movement work in close relationship with the tertiary neurosciences research team. Patients may be invited to participate in research work if suitable.
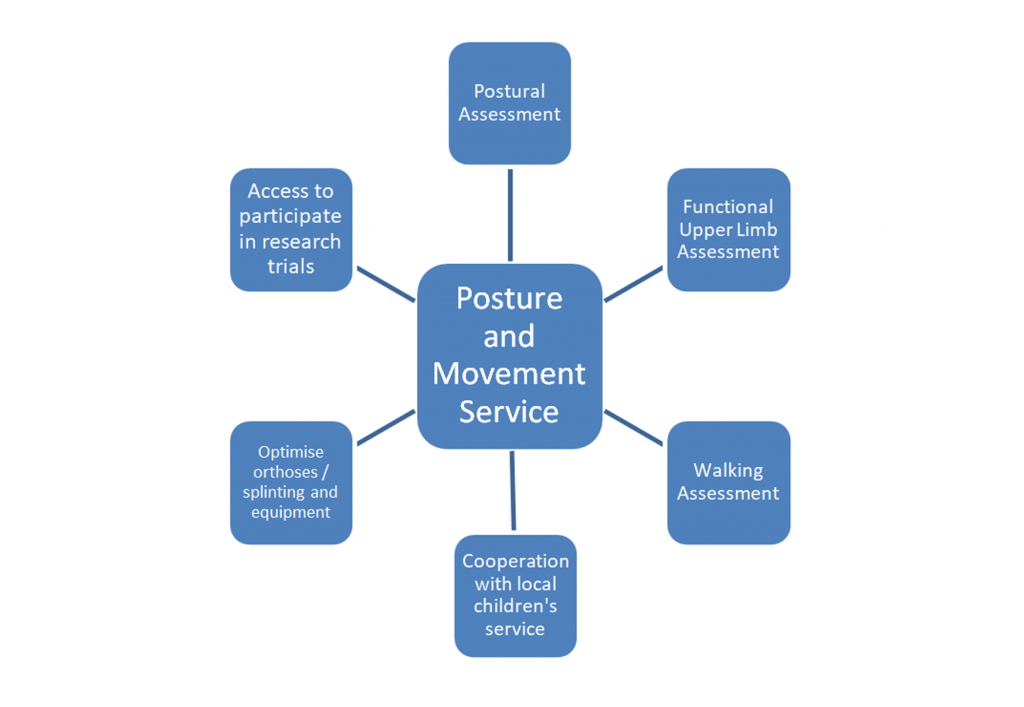
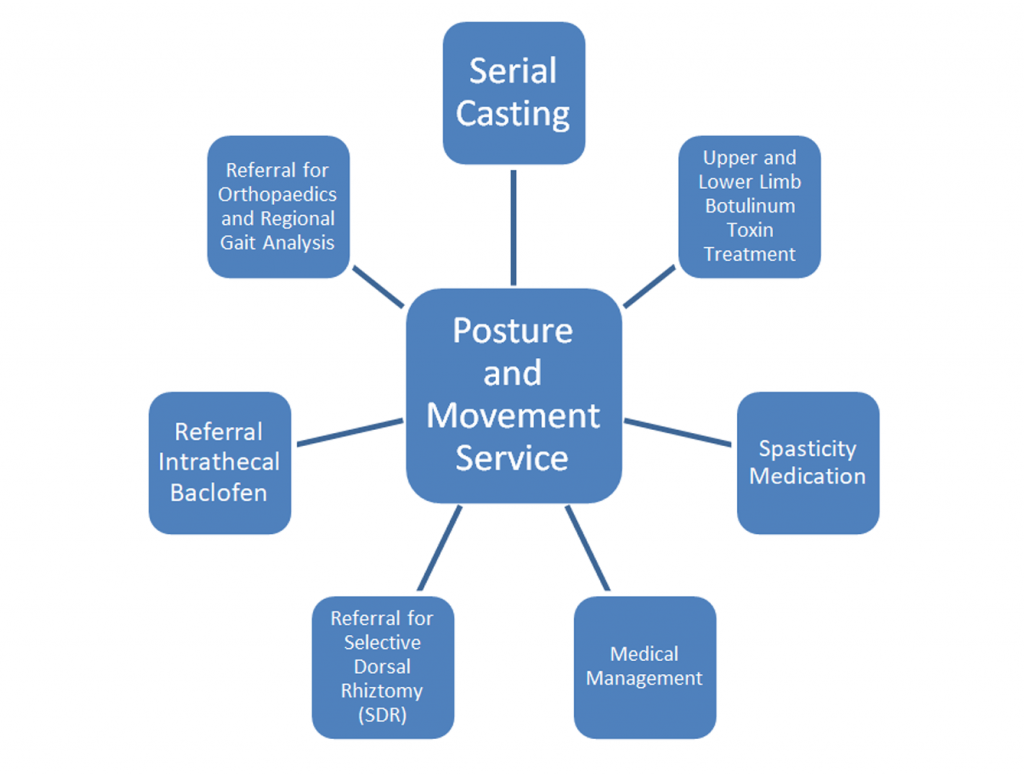
The diagrams below show possible assessments and treatments available.
Assessment
Treatment / Referral
Postural assessment
In this clinic we consider all aspects of your child’s care. Emphasis is placed on current mobility, equipment, orthotics/splints, therapy programmes and previous treatments including surgery. Parents and children are encouraged to discuss any concerns with the clinic team.
Following this discussion, the team will assess your child’s movement and mobility (transfers and walking). Where walking is being assessed, the child will be asked to walk with and without their usual aids and orthoses/splints.
The team will discuss the findings and treatment options to help with your child’s difficulties. Before the appointment your child’s local therapy team will be contacted and asked to provide information about therapy goals, concerns, orthotics/splints and equipment to date.
A written report is sent to the parents, referrer and an agreed circulation list after the assessment.
Follow up will be arranged depending on the assessed needs of the child.
Upper Limb Clinic
Children who require further upper limb assessment will then be seen in this clinic.
Prior to assessment parents and children are asked to complete a detailed questionnaire regarding how they use their arm, any splints worn, and current parental concerns.
Our assessments of upper limb function will help guide your child’s treatment plans which we organise in conjunction with your local therapy team. We focus on current, relevant goals for your child to maximise his/her ability in two-handed tasks.
Walking Assessment Clinic
Prior to assessment parents and children are asked to complete a detailed questionnaire regarding mobility, walking aids, splints, and current parental concerns.
Children then have a video assessment of walking in and out of their splints and where appropriate using their aids. This is followed by a detailed assessment of joint movement, muscle tightness and function. The assessments are then reviewed and a management plan is agreed with the family.
Botulinum Toxin Procedure Clinic
Following assessment children may be invited to return for targeted intramuscular injections. The injections are carried out under local anaesthesia and/or sedation. You can find out more information about the botulinum toxin procedure here.
Physiotherapy follow-up post Botulinum toxin treatment
Children who are walking will have their walking re-assessed 6-8 weeks post botulinum toxin treatment. The physiotherapists in this clinic will complete all necessary assessments to review the outcome of your child’s treatment. Prior to this clinic parents and the child’s local therapy team are also asked about the treatment outcomes.
Joint Orthopaedic Clinic
Children who may require management from the orthopaedic team will be seen in this clinic where there is advice available from a consultant paediatric neurologist, Consultant in Paediatric Neurodisability, consultant orthopaedic surgeon and specialist Physiotherapist.
Contact: Karen Armstrong-Jordan
Secretary to Dr Anita Devlin and Dr Yasmin de Alwis
Office Block 1, Level 2, Clinical Resource Building, RVI
Tel: 0191 2821385 (Option No. 1) / Ext. 25240