On this page
What is preimplantation genetic diagnosis?
Preimplantation genetic diagnosis (PGD) is an IVF-based treatment that may be suitable for some women who are at risk of transmitting a mitochondrial DNA mutation to their children.
PGD is for mitochondrial DNA disease is based on the principle that the level of mutated mitochondrial DNA can vary widely between eggs produced by a women who carries a mixture of mutated and normal mitochondrial DNA.
PGD is only suitable for women who are expected to produce some eggs with low levels of mutated mitochondrial DNA.
What does PGD involve?
PGD involves undertaking a series of injections to stimulate the ovaries to grow multiple eggs. A number of ultrasound scans are performed to monitor the ovaries during the stimulation phase. When they are at the correct stage, the eggs are harvested using a fine needle to aspirate them from the ovaries.
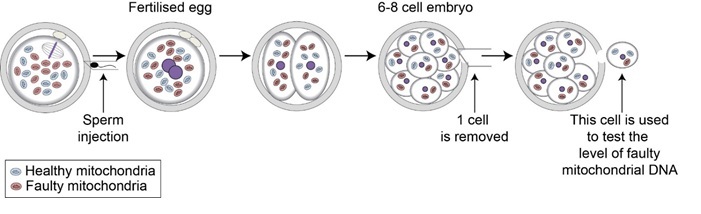
The eggs are fertilised by injecting the male partner’s sperm using a technique known as intra-cytoplasmic sperm injection (ICSI). Approximately 60-70% of eggs fertilise following ICSI. Those that fertilise normally are grown in the lab for 3 days. By this time good quality embryos contain between 6 and 10 cells. For PGD, we remove one of these cells for genetic testing. The genetic tests will enable us to identify the embryos with the lowest levels of mutation.
The embryos are grown for a further 2 days. By then (5 days after fertilisation), the best quality embryos will have developed to the blastocyst stage. Development to this stage is essential for embryos to implant in the womb.
Taking account of the level of mutation and the embryo quality, either one or two embryos will be selected and transferred to the womb. This involves placing the selected embryos into a tube, which is then passed through the cervix and the embryos are gently expelled into the womb.
If suitable embryos remain, they are frozen and stored for future treatment
Before deciding to proceed to embryo transfer, the couple will have a further discussion with their clinical team.
Preimplantation genetic diagnosis (PGD)
How likely is it that PGD will result in a pregnancy?
Unfortunately, some women do not produce eggs with sufficiently low levels of the mitochondrial DNA mutation. In these cases a new treatment known as mitochondrial donation may be suitable.
If embryos are replaced, the pregnancy rate following PGD is similar to conventional IVF treatment. In our clinic, the pregnancy rate after one cycle of IVF treatment is 40%.
This increases to 63% after three cycles of treatment. However, a number of factors can affect the outcome, in particular the success rate declines markedly as women get older, from the age of 35 years onwards.
How likely is it that PGD will prevent transmission of mitochondrial DNA disease?
The evidence to date suggests that PGD provides a reliable approach to reducing the risk of mitochondrial DNA disease. However, this is dependent on the levels of mutated and normal mitochondrial DNA contained in the embryo(s) selected and replaced in the womb.
In all cases reported so far, the mutation level in the tested cell was similar to that measured in the new-born baby or in the cord blood. There is one report where this was not the case, however, it is not clear whether this was due to an error in the levels measured in the embryo.
To minimise the risk of such an error, our PGD programme is run in collaboration with an accredited mitochondrial genetics lab at the Welcome Trust Centre for Mitochondrial Research.
Useful links
HFEA – Mitochondrial donation treatment