On this page
What is mitochondrial donation?
Mitochondrial donation is an IVF based technique to replace the faulty mitochondrial DNA in the patient’s eggs with healthy mitochondrial DNA from a donor egg.
At Newcastle Fertility Centre we offer a procedure called pronuclear transfer (PNT) for mitochondrial donation. We have performed extensive research on this technique.
We only offer this treatment to patients with mitochondrial disease where other treatments, such as PGT-M, are unsuitable.
We do not have a license to offer this treatment to patients who have a fertility problem without mitochondrial disease.
Pronuclear transfer (PNT)
What does PNT involve?
To perform PNT, we will need multiple eggs from the patient and from a donor who does not carry a mitochondrial DNA mutation.
Both women will undertake a series of injections to stimulate the ovaries in order to grow multiple eggs.
A number of ultrasound scans are performed to monitor the ovaries during the stimulation phase. When they are at the correct stage, the eggs are harvested using a fine needle to aspirate them from the ovaries.
The patient’s eggs will generally be collected in advance and will be cryopreserved using a technique known as vitrification. The patient’s eggs are taken out of storage on the day of the donor’s egg collection. Both sets of eggs are then fertilised by injecting sperm from the patient’s partner, using a technique known as intra-cytoplasmic sperm injection (ICSI).
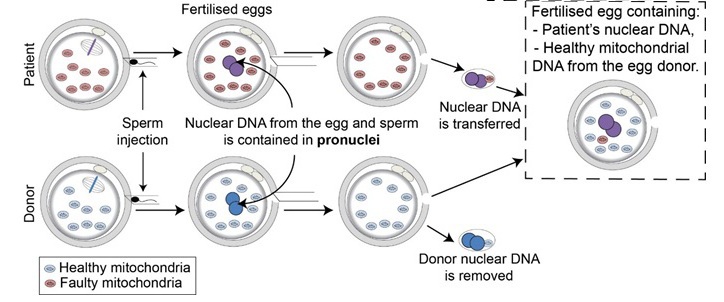
Approximately 6-8 hours after sperm injection we will remove the nuclear DNA from the egg and the sperm, which are contained in the pronuclei. The pronuclei from the patient’s egg are then allowed to fuse with the donor egg. This results in a reconstructed egg, which contains the nuclear DNA from the patient and her partner and mitochondrial DNA from the unaffected donor (see diagram).
The PNT embryos will be grown in the lab up to day 5 after the PNT procedure. We will then select the best quality embryo(s) for use in treatment. Either 1 or 2 embryos will be replaced in the womb and any remaining good quality embryos will be frozen and stored for future use.
How likely is it that PNT will result in a pregnancy?
Because PNT is a new treatment we do not yet have enough data to estimate the chance of pregnancy. However, we have performed extensive research on PNT and our findings indicate that PNT is compatible with the establishment of a viable pregnancy.
How likely is it that PNT will prevent transmission of mitochondrial DNA disease?
When we perform PNT, a very small amount of mitochondrial DNA is co-transferred with the pronuclei (see diagram above). This means PNT embryos may contain a small amount of mutated mitochondrial DNA.
While we make every effort to minimise this, our research suggests that it may, on rare occasions, increase as the embryo develops in the womb.
We cannot yet guarantee that PNT will eliminate the risk of disease. We therefore recommend that patients undergoing PNT consider antenatal screening for mitochondrial disease for reassurance.
Factors that influence the outcome of PNT treatment
As with all IVF treatments, the outcome of PNT treatment is affected by a number of factors. These include the quality of the sperm and the number and quality of the eggs we obtain. In particular, the success rate declines markedly as women get older – from the age of 35 years onwards. We therefore recommend that, where possible, patients have their eggs frozen and stored before the age of 35 years. This is not always possible, but it is advisable.
Useful links
HFEA – Mitochondrial donation treatment