On this page
Introduction
This leaflet is for pregnant women with a suspected finding of a spina bifida on antenatal ultrasound examination. The leaflet should only be given with consultation by a senior obstetrician, fetal medicine specialist or neurosurgical specialist.
What is spina bifida?
Spina bifida occurs in approximately 1 in 1000 babies.
This is a condition in which some of the spinal bones (vertebrae) and part of the spinal cord have not formed completely. As a result of this, some of the spinal cord and nerves come out through a hole in the baby’s back, often covered by the protective membrane, or sac, that surrounds the spinal cord and nerves. This is also referred to as an open spina bifida, myelomeningoecele or spina bifida aperta.
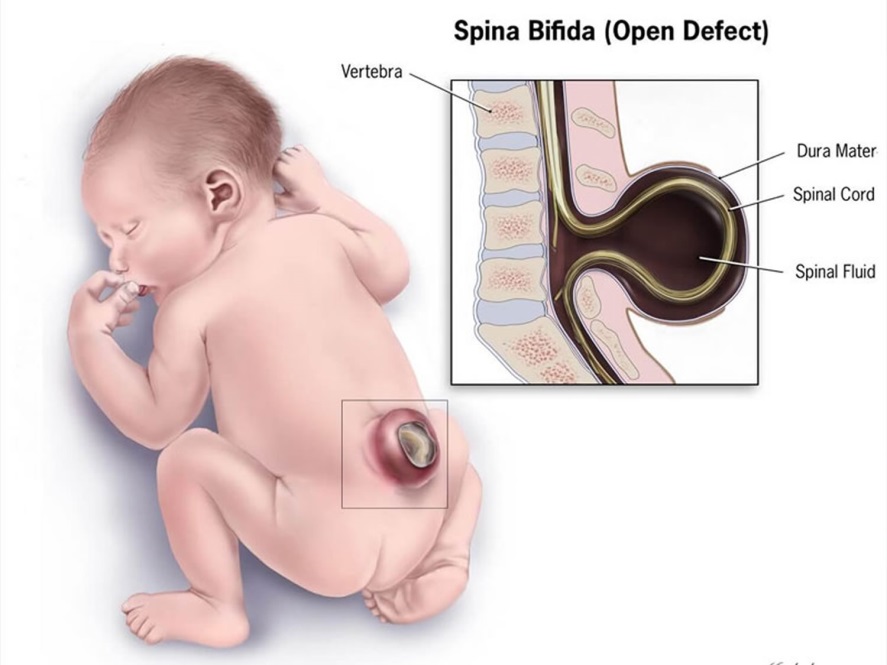
Another form of spina bifida (spina bifida occulta), occurs when the spinal cord and nerves do not fully form but the overlying skin is present forming a protective barrier. This is also referred to as a closed spina bifida. Most of the information explained in this leaflet refers to open spina bifida.
What causes spina bifida?
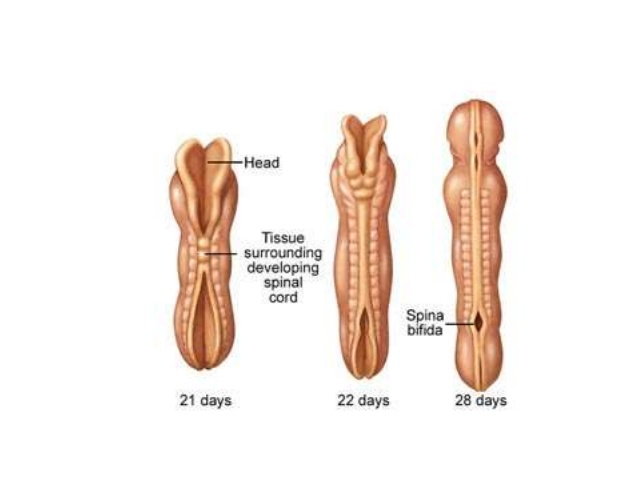
Spina bifida is a form of neural tube defect. The neural tube is a structure that forms the brain and spinal cord at a very early point in the pregnancy (the first four weeks). This structure closes centrally and then extends, closing like a zip, to the head and bottom ends of the early developing fetus. When the tube does not effectively close at the bottom end, a spina bifida occurs.
It is not fully understood why this happens however it most likely due to a number of genetic and environmental factors. The most common recognised cause of spina bifida is low folic acid levels in the mother. For this reason, you would be advised to take a higher dose of folic acid (5mg as opposed to the standard 0.4mg) in any future pregnancies.
In most cases of spina bifida, this occurs as an isolated problem, however 1-2% of the time an additional underlying chromosomal problem may be present. In most cases of chromosomal abnormality, more problems will be seen on the ultrasound scan. Your doctor will discuss the option of a diagnostic test called an amniocentesis which will look at the baby’s chromosomes in more detail.
What does it mean for my baby?
The exact effect of this condition on your baby is difficult to predict however a range of possible problems are associated with spina bifida (particularly open spina bifida) because of the exposure and possible damage to the spinal cord and nerves. Unfortunately, it is likely that the baby will have some damage to the nerves at and below the level of the spinal lesion.
In most cases there is an effect on the baby’s long term control of bowel and bladder function, however with planned insertions of a urinary catheter and rectal suppositories, many children and adults will be “socially continent”. This means they can learn to empty their bowel and bladder at appropriate times. Catheterisation and insertion of suppositories is something parents would perform in early childhood but most children will learn to perform themselves at some point later in childhood.
The extent of the effect on the child’s ability to walk is very difficult to predict before they are born, however higher spinal lesions are more likely to be associated with mobility problems. It is common for children to have some weakness in the muscles of the legs and feet, and those who are fully independently mobile when they are young may choose to use walking aids or a wheelchair as they grow up in order to be more easily mobile.
A further consideration is that spina bifida will often have an effect on sexual function.
An additional problem often associated with open spina bifida is an abnormality of the back of the brain called a Chiari malformation. A Chiari malformation can lead to restriction of the flow of cerebrospinal fluid around the base of the brain and the top of the spinal cord and can sometimes lead to fluid build-up inside the spinal cord (a syrinx) or within the brain (ventriculomegaly). Ventriculomegaly may be mild and not cause any problems but if the ventricles continue to enlarge over time then it may be necessary to drain the fluid by doing a small operation to insert a ventriculoperitoneal (VP) shunt. Just over half of children with spina bifida will need a shunt. If your baby needs this procedure then a neurosurgeon will explain it to you in detail. There are some potential complications of VP shunts which would be discussed before surgery.
Other common problems associated with spina bifida are a scoliosis (curvature of the spine) and talipes (club foot). Your fetal medicine specialist may be able to see these problems on the ultrasound scan or they may be evident following the baby’s birth.
As explained above, in a small number of babies, spina bifida occurs because of an underlying chromosomal abnormality. If a chromosomal problem is confirmed on amniocentesis then there may further problems not already mentioned in this leaflet.
What happens now?
You will be offered an appointment with a consultant in the fetal medicine unit to confirm the diagnosis and to review your baby for the presence of any additional problems. Based on these findings the doctor will describe the possible outlook for your baby. The option of an amniocentesis will be discussed with you. It is entirely your decision if you would like to proceed with this test or not.
We appreciate that this will be an extremely stressful time for you and your family, particularly given the large amount of information we are asking you to understand in a short amount of time.
Following your consultation, you will be offered more appointments with a Neurosurgical and Neonatal Consultant to discuss the postnatal care of the baby in more detail. You will also be offered additional scans throughout your pregnancy to review the growth and wellbeing of your baby and to measure the fluid within the brain and the size of your baby’s head. The purpose of these appointments will also be to ensure we have answered all your questions and you feel prepared for the birth of your baby.
For many women, their partners and families, the diagnosis of spina bifida causes a significant concern for the long term care for the child. In this situation, many will consider the option to terminate the pregnancy. We appreciate that this must be an extremely difficult and individual decision. Your doctor will discuss this option with you in more detail. There is no rush to make this decision and women and their partners may take some time considering their options.
How should I give birth to my baby?
The safest place for your baby to be delivered if you live in the North East or Cumbria is at the Royal Victoria Infirmary (RVI), Newcastle upon Tyne, where specialist neonatal and paediatric neurosurgical teams are based. During the course of your pregnancy, the Fetal Medicine team will organise transfer of your maternity care from your local hospital to the RVI. Delivery, often by induction of labour, is usually arranged around 39-40 weeks gestation to ensure your baby arrives on a planned date and at the RVI. This will ensure all the medical teams involved are present at the birth and that there is an available cot in Neonatal surgical unit. Occasionally the planned date is changed due to other emergencies in the department meaning cots/incubators become unavailable for a short time.
If you go in to labour sooner than expected you should attend your closest hospital for assessment.
All of your usual pregnancy care should still take place and it is important to still arrange to see your community midwife for routine antenatal appointments.
We recommend aiming for a vaginal delivery if possible. There is no known benefit of Caesarean birth in most cases of spina bifida. If however, there is a large accumulation of fluid within your baby’s head causing them to have an enlarged head, vaginal birth may be difficult and we would recommend a Caesarean section delivery.
What happens after the birth?
We would expect your baby to be generally well at birth, to breath and to cry. A team of doctors and nurses will be present when your baby is born. They will place the baby on an infant warmer with resuscitation equipment (resuscitaire) and cover the exposed area on the baby’s backs with a protective film to ensure that it is not damaged. They will then transfer the baby to the neonatal unit for assessment and preparation for surgery.
Because of this it will not be possible to hold your baby immediately after birth but the neonatal doctors will bring the baby close to you before they take the baby to the neonatal unit. After the baby is taken to the neonatal unit, they will undergo a series of investigations such as blood tests and an MRI. You will be informed of their progress and your midwife will check with the neonatal team to find out when it is possible for you to go to the neonatal unit to see your baby.
Surgery to repair the defect in the baby’s back occurs within the first few days of life. The neurosurgical team will discuss the details of the surgery and the recovery time with you in more detail.
Some cases of spina bifida can be repaired during the pregnancy, before the baby is born (antenatal surgery). The Fetal Medicine team will assess if your baby would be eligible for this procedure, and if so, will discuss the option, as well as the risk and benefits of earlier spina bifida repair with you.
Can I stay with my baby?
Crawford House is situated within the grounds of the RVI and provides a “Home from Home” supporting families with children being treated at the RVI. Accommodation is provided for those who live outside of Newcastle and is provided free of charge by the registered charity, The Sick Children Trust. The house is available 365 days a year and has 23 private family bedrooms. There is a fully- equipped kitchen, dining area, playroom and living room alongside bathrooms and laundry facilities. Rooms are allocated on a priority basis and unfortunately cannot be pre booked before delivery. Once you are discharged from the Maternity Unit, accommodation can be booked.
For further information
For further information please contact:
Fetal Medicine Department,
Royal Victoria Infirmary
(0191) 2825837
Monday –Friday 9-5pm
Be sure to ask questions to the doctor supplying you with this leaflet and make a note of any questions you would like to ask at your next Fetal Medicine Unit appointment.
Antenatal Results and Choices
0845 077 2290 or 0207 713 7486 via mobile
North of Tyne Patient Advice and Liaison Service (PALS)
0800 0320202
Monday to Friday 9.00-4.30pm (answer phone out of hours)
Email: [email protected]
Resource Information
Information produced by Lesley Walker (Fetal Medicine Lead) Date July 2019
Revised by Lin Foo (consultant 26/09/2023)
Review date: Sept 2026