On this page
Cleft lip and palate
Who is this information aimed at?
This leaflet is aimed at pregnant women with a finding of a cleft lip and or palate on ultrasound examination. The leaflet should only be given with a consultation with a senior obstetrician, fetal medicine specialist or cleft nurse specialist.
What is a cleft lip/palate?
In early fetal development, different parts of a baby’s face develop separately and then join together. If some parts do not join properly, the baby is born with a facial cleft. A cleft lip can range from a little notch in the coloured part of the lip to a complete separation of the upper lip which can extend up and into the nose. This can affect one side of the mouth (unilateral) or both sides (bilateral), and can be complete (meaning the cleft goes up into the nose) or incomplete.
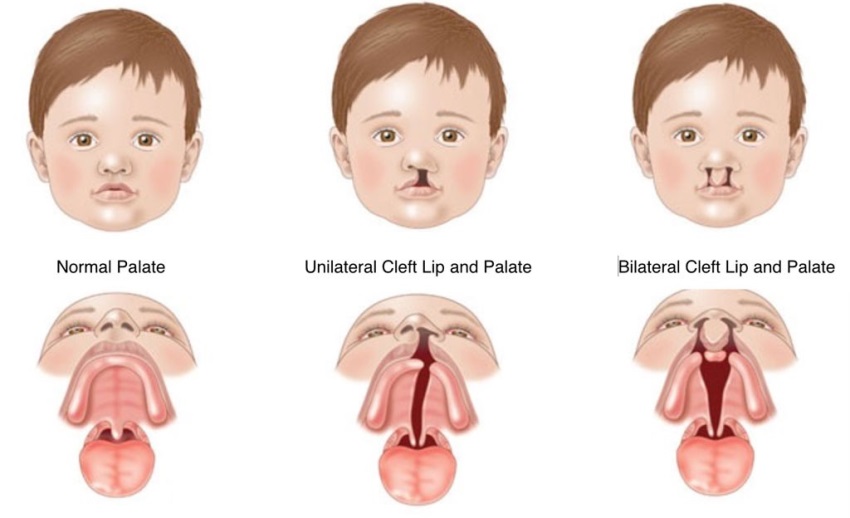
A cleft palate is a gap in the roof of the mouth. The back of the palate (towards the throat) is called the soft palate, and the front (towards the lips) is called the hard palate. A cleft can affect the soft palate or both the soft and hard palate.
Babies with a cleft lip have an associated cleft palate in 50% cases.
How is it diagnosed?
This condition is often diagnosed during pregnancy but soft palate clefts are extremely difficult to visualise on ultrasound scan and cannot be ruled out until a neonatal examination is performed following delivery. You will usually be offered a 3D/4D scan so that you can see your baby’s face in more detail.
What causes it?
A cleft lip and/or palate are the most common craniofacial abnormality (a problem related to the skull and face) which babies can be born with approximately 1 in 700 pregnancies. It is believed to be due to a number of complex genetic and environmental factors and is not something that could have been prevented. It is known to be more common if another family member has also been affected however will occur without any family history in most cases. It is rare for facial clefts to be due to an underlying chromosomal or genetic abnormality such as trisomy 13 or 18 or Treacher Collins Syndrome. If it occurs in isolation, this risk is likely to be no more than 1% but we can offer an invasive test such as an amniocentesis to check your baby’s chromosomes. (See separate information leaflet).
What does it mean for your baby?
During the pregnancy you will be seen regularly by a specialist nurse to ensure that you feel prepared for managing the baby following delivery. Babies born with facial clefts are expected to be well at birth and this should not affect how, where or when the baby is delivered. The most noticeable difference following delivery is that your baby will need some additional support with feeding. Many babies with facial clefts will have difficulty latching on and creating a seal so your specialist nurse will explain how to use specialist bottles for feeding. Breast milk can be expressed and used in these bottles if you wish.
How is it treated?
Repair of the lip usually occurs between 3-4 months of age and the palate between 10-12 months. This is a time that is believed to be safest and have the best outcome for the baby. Your specialist nurse will show you pictures of babies with similar facial clefts and their appearance following surgical repair.
Children with a facial cleft will have ongoing outpatient clinic appointments as they get older particularly with ear, nose and throat (ENT) specialists and speech and language specialists. Some of these children with a palatal cleft may require orthodontic work in childhood.
Who else can I contact for support?
Be sure to ask any questions to the doctor supplying you with this leaflet and make a note of any questions you would like to ask at your Fetal Medicine Unit appointment. You will be given contact details for the cleft nurse specialist and another helpful resource is the Cleft Lip and Palate Association website.
For further information
For further information please contact:
Fetal Medicine Department,
Royal Victoria Infirmary
(0191) 2825837
Monday –Friday 9-5pm
Be sure to ask questions to the doctor supplying you with this leaflet and make a note of any questions you would like to ask at your next Fetal Medicine Unit appointment.
Antenatal Results and Choices
0845 077 2290 or 0207 713 7486 via mobile
North of Tyne Patient Advice and Liaison Service (PALS)
0800 0320202
Monday to Friday 9.00-4.30pm (answer phone out of hours)
Email: [email protected]
Resource Information
Information produced by Ruth Thompson and Lesley Walker (Fetal Medicine Clinical Lead)
Date 22/08/2019
Updated by Angela Lightfoot: 21/7/2023
Review date: July 2026