On this page
Who is this information leaflet aimed at?
This leaflet is aimed at pregnant women with a confirmed parvovirus infection. The leaflet should only be given with a consultation with an experienced obstetrician.
What is parvovirus?
Parvovirus B19 is a common infection that usually affects children and causes a mild illness and a facial rash. It is often called slapped cheek disease. The risk of infection is greater in people who have frequent contact with children such as teachers, and those with school age children.
Once you have had the infection you are immune and will not get it again and therefore this would not be a risk to your pregnancy. 60% of adults have had the infection and are immune. For women who develop the infection for the first time during pregnancy, the symptoms can be very mild and they may hardly be aware that they have been infected.
Up to 5% of women will develop parvovirus infection during pregnancy, most of these women will deliver a healthy baby.
What does it mean for your baby?
If a woman develops a parvovirus infection during pregnancy there is a risk (about 30%) of the baby also developing the infection. Parvovirus infection can be dangerous for developing babies, as the virus can cross the placenta and affect the way the baby’s red blood cells develop. As a result, a small percentage of infected babies will develop anaemia (low blood count). In the most serious cases, this can affect how the baby’s heart functions and may cause miscarriage or stillbirth if it is not treated. The risk of serious complications is small but is probably higher if the infection occurs earlier in your pregnancy (before 20 weeks gestation.)
The risk of the baby developing other problems related to the infection is small.
How is it diagnosed?
Parvovirus is not something that is routinely tested for during pregnancy. If you suspect that you have come into close contact with a person with the infection then speak to your midwife. Your midwife can organise for the routine blood sample taken early in your pregnancy to be tested to check your immunity (previous exposure) to the virus. If there is no evidence of immunity then she will take a blood test 2-4 weeks after your exposure that will check if you have recently been infected.
The other reason that you may be offered a test is if your baby appears to show signs of a possible parvovirus infection during an ultrasound scan.
What are the signs of anaemia in the baby during the pregnancy?
In some babies who develop anaemia, the mother may feel less movements than normal, however ultrasound scans are usually a more reliable way of assessing for anaemia in the baby. During your scans, your doctor will measure the speed of blood flow in a blood vessel in the baby’s head called the middle cerebral artery (MCA). If this is unusually fast, it may be because the baby is anaemic.
Other signs of more significant anaemia are when the baby develops fluid in its chest or abdominal cavity. In this situation, the baby would need treatment whilst still in your womb or after delivery.
How is it treated?
Most women and babies will need monitoring with regular ultrasound scans. These will occur every week and will be performed by a specialist doctor in your local hospital or at the Fetal Medicine Department at the Royal Victoria Infirmary. You will require these regular scans for up to 10 weeks after a confirmed infection.
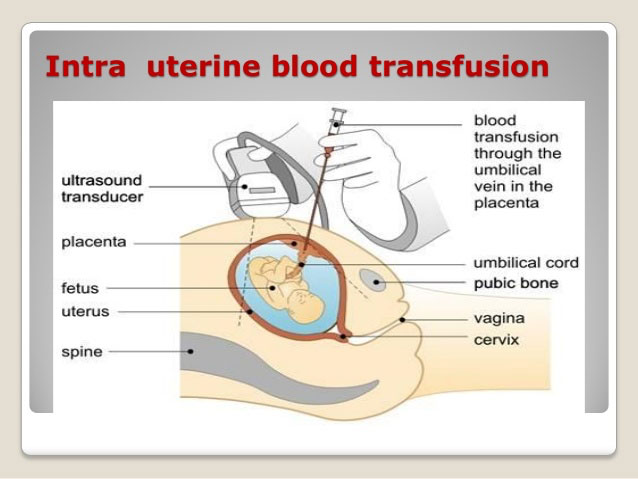
Only a small number of babies need treatment for anaemia during the pregnancy. This involves giving the baby blood transfusion while still in the womb. This is a very specialist procedure that will be performed in the Fetal Medicine Department. If a blood transfusion is needed, often no other treatment is needed after that.
What happens next?
If you have had a blood test that confirms you have had a recent parvovirus infection then your doctor will discuss your case with you and refer you to the Fetal Medicine Unit at the Royal Victoria Infirmary. You will be offered specialist scans to assess your baby for signs of anaemia.
For further information
For further information please contact:
Fetal Medicine Department,
Royal Victoria Infirmary
(0191) 2825837
Monday –Friday 9-5pm
Be sure to ask questions to the doctor supplying you with this leaflet and make a note of any questions you would like to ask at your next Fetal Medicine Unit appointment.
Antenatal Results and Choices
0845 077 2290 or 0207 713 7486 via mobile
North of Tyne Patient Advice and Liaison Service (PALS)
0800 0320202
Monday to Friday 9.00-4.30pm (answer phone out of hours)
Email: [email protected]
Resource Information
Information produced by Lesley Walker (Fetal Medicine Clinical Lead)
Date July 2019
Updated by Angela Lightfoot: 21/07/2023
Review date: July 2026