5 July 2023 marks 75 years of the National Health Service.
Treating over a million people a day in England, the NHS touches all of our lives. When it was founded in 1948, the NHS was the first universal health system to be available to all, free at the point of delivery. Today, nine in 10 people agree that healthcare should be free of charge, more than four in five agree that care should be available to everyone, and that the NHS makes them most proud to be British.
Treating 1.3 million people a day the NHS has been a constant presence throughout our lives. As we mark 75 years of the NHS on 5 July 2023, we’re looking back on the history and achievements of the NHS in Newcastle.
1948 – The NHS is born
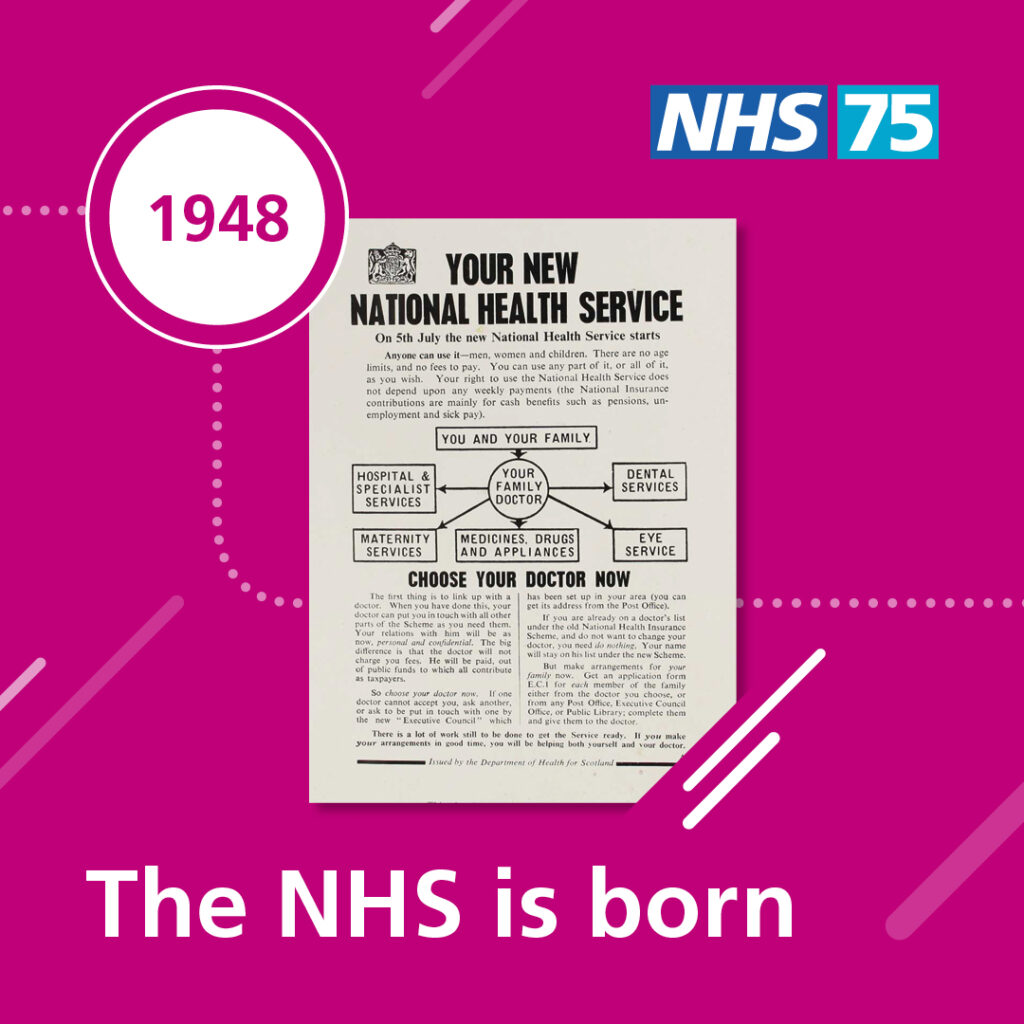
The NHS was launched on 5 July 1948 by Health Secretary Aneurin Bevan, as the first universal health system, free to all, at the point of need. Different healthcare services were brought together and this improvement in access made a significant difference to many, especially where specialist consultant services had been limited.
On this day, Princess Mary Maternity Hospital and the Newcastle upon Tyne Dental Hospital combined with the Royal Victoria Infirmary (RVI) into The United Newcastle upon Tyne Hospitals.
The RVI was one of 36 teaching hospitals nationally, providing teaching and research to students at Newcastle University.
Tyneside was also served by Newcastle Eye Hospital, Newcastle General Hospital and Fleming Memorial Hospital, under the Newcastle Hospital Management Committee.
1950s – NHS in demand

As the NHS developed, so did demand for services. Hospitals were under pressure and patients’ expectations were growing.
In 1952, a one-shilling (5p) charge for prescriptions and a 20 shillings (£1) charge for dental treatment were introduced.
During the 1950s, children were commonly treated in adult wards. Parents were often only allowed to visit for an hour on Saturdays and Sundays, with some even discouraged from visiting at all. Paediatricians Sir James Spence in Newcastle and Alan Moncriff at Great Ormond Street pioneered daily visiting for children, which was gradually introduced over the next decade.
At the time, cases of diphtheria and polio were high. In 1958, the first mass vaccination programme was introduced to under 15s, leading to a dramatic reduction in both diseases.
1960s – Innovation
In the 1960s, as vaccination programmes began, diseases such as polio were reducing, but this was met with a new challenge of an increase in chronic disease.
The decade saw a noticeable rise in medical knowledge and significant advances in treatment.
In 1962, ‘The Hospital Plan’ brought in a new era of hospital buildings. Newcastle’s teaching hospital received 1,200 additional beds and specialist services were split between Newcastle General Hospital and a new hospital to be built on Freeman Road.
Joint replacement surgery was introduced and, in a pioneering move, organ transplantation became a reality as Newcastle surgeons carried out the first kidney transplant in 1963.
In the 1960s, Newcastle psychiatrist Professor Sir Martin Roth’s ground-breaking research differentiated between groups of mental health disorders affecting older people, which included new guidance for assessing patients and inspired the establishment of geriatric psychiatry as a speciality.
1970s – Hospital remodelling
In 1972, Newcastle University, the RVI Board and Regional Hospital
Board agreed to form a joint university hospital management committee, encompassing all hospitals in Newcastle and forming the Newcastle Area Health Authority.
Hospital services were remodelled and all of the teaching hospitals, including the Royal Victoria Infirmary, Princess Mary Maternity Hospital and the dental hospital began to combine. In 1977, a new purpose-built dental hospital and school were constructed on Richardson Road.
In 1972, the construction of Freeman Hospital began, with the first patients admitted in 1977. This allowed the transfer of specialist services, such as heart and lung, orthopaedics, ear nose and throat, renal and urology from hospitals across the north east.
Records show the first clinical trial in Newcastle’s hospitals was registered in 1975.
1980s – Pioneering treatments

The NHS in Newcastle pressed ahead with pioneering medicine, as teams at the Royal Victoria Infirmary began to develop assisted fertility treatments.
In 1985, the heart transplant programme started at the Freeman Hospital and, in 1987, medical history was made when Kaylee Davidson became the first baby in the country to have a successful heart transplant.
Since then, Newcastle’s transplant team has celebrated many milestones and Innovations, including the first successful single and double lung transplants in Europe, in 1987 and 1990 respectively.
In 1987, Fleming Memorial Hospital for Sick Children closed and services were moved to the Royal Victoria Infirmary.
Treatment of cancer became a priority for the NHS, with breast and cervical cancer screening launched in 1988.
1990s – Newcastle Hospitals is created

During the mid-1990s, it became apparent that demands on the NHS were increasing.
Between 1991 and 1995, hospital providers became NHS Trusts, enabling independent management of budgets and organisations, plus the freedom to arrange healthcare to meet the needs of local communities.
To bring together resources and expertise, in April 1998 the Royal Victoria Infirmary and Associated Hospitals NHS Trust and The Freeman Group of Hospitals NHS Trust merged to form The Newcastle upon Tyne Hospitals NHS Trust.
In 1991, the life-changing falls and syncope service opened at the RVI, which remains the largest of its kind in Europe. The service investigates, diagnoses and helps manage blackouts and loss of consciousness causing falls, particularly in older patients.
2000s – Transforming Newcastle Hospitals

In 2000, the NHS Plan was launched to improve service standards across the country and give patients greater choice.
Most of Newcastle’s specialist services were provided at the General Hospital on Westgate Road or the RVI, and a long-term review led to some significant changes.
After years of major construction and development, the Northern Centre for Cancer Care and Renal Services opened in 2004 and the New Victoria Wing at the RVI opened in 2009.
In 2000, the International Centre for Life was launched, including the Newcastle Fertility Centre. The first IVF baby in the country was born as a result of the centre’s ground-breaking work.
Newcastle Hospitals became an NHS foundation trust in 2006, governed with the involvement of local people and staff, and giving greater independence over service planning and delivery.
In 2009, Newcastle Surgical Training Centre was unveiled, providing a unique facility for education and training in Newcastle and beyond.
2010s – Major developments in Newcastle

Significant developments continued in this decade, when children’s services from sites across Newcastle were brought together in a state-of-the-art new building at the RVI – the Great North Children’s Hospital, which opened in 2010.
Also in 2010, Newcastle’s emergency department relocated across the city to establish the Great North Trauma and Emergency Centre.
In 2011, the Institute of Transplantation opened at Freeman Hospital – the first advanced healthcare facility of its kind in the UK dedicated solely to organ transplantation.
In the same year, Newcastle’s Professor Roy Taylor’s research showed that type 2 diabetes could be reversed through a low-calorie diet and weight loss programme, which is now a clinically-proven way to tackle early type 2 diabetes used across the NHS.
In 2014, Newcastle Hospitals introduced revolutionary robotic surgery and now provides this surgery for more specialties than any other hospital in Europe.
In 2018, and following 20 years of development and successful trials, a cancer drug developed by Newcastle clinicians was approved for Europe-wide use.
2020s – Progress in challenging times

The early 2020s were some of the most challenging years for the country and the NHS, as the Covid-19 pandemic hit.
In January 2020, Newcastle Hospitals treated the UK’s first Covid patients and, as the pandemic progressed, set up the UK’s only integrated Covid hub to boost the region’s response.
A legacy of the Covid hub, the North East Innovation Lab continues to work with developers from across the globe, to assess cutting-edge diagnostic tests to tackle a range of health issues.
Newcastle was also instrumental in the national Covid vaccination programme, through early research into vaccine effectiveness and then organising vaccine delivery through large centres across the region.
Against this backdrop, service improvements continued.
In 2021, the Northern Centre for Cancer Care, North Cumbria opened at Cumberland Infirmary, supporting patients to receive cancer treatment closer to home.
To help tackle waiting list backlogs caused by the pandemic, the Westgate Cataract Centre was launched in 2021 and a dedicated £24m day treatment centre opened at Freeman Hospital in 2022, providing capacity for 7000 additional procedures each year.
A number of ‘firsts’ saw the RVI’s maternity unit became the first in the UK to use climate-friendly gas and air, and Grace Westwood became the first child in the UK to have a mobile Berlin Heart device fitted while waiting for a heart transplant at the Freeman Hospital.
In 2021, the first series of Geordie Hospital aired on Channel 4, showcasing the very best of Newcastle Hospitals.
In 2022, research led by Newcastle Hospitals found that an antiseptic drug is as good as antibiotics for preventing recurrent urinary tract infections, which could help find vital alternatives to antibiotic treatment.
