On this page
Who is this information leaflet aimed at?
This leaflet gives general information about Congenital Diaphragmatic Hernia (CDH). If there are any changes for your individual circumstances then these will be explained during your consultation with a senior obstetrician or Fetal Medicine specialist.
What is Congenital Diaphragmatic Hernia (CDH)?
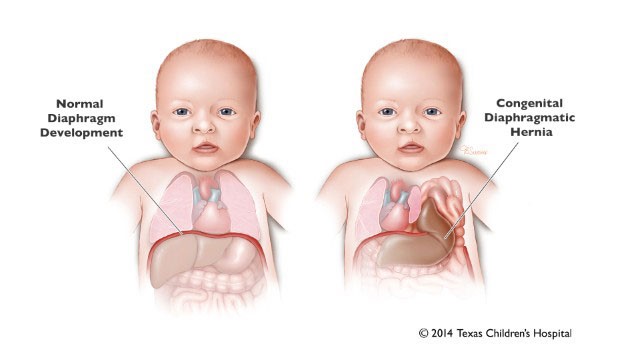
‘Congenital’ refers to a condition that a baby is born with. ‘Diaphragmatic’ refers to the curved muscle which sits between the chest and the abdomen. ‘Hernia’ is a term used to describe a bulge or protrusion of an organ through a structure or muscle that usually contains it.
The diaphragm muscle helps us breathe and to separate the chest from the abdominal contents. A congenital diaphragmatic hernia (CDH) may form on the left or right side if that part of the muscle does not develop completely. This leaves a hole which allows some of the abdominal contents to move up into the chest cavity. This hole will have formed between the 7th to 12th week of pregnancy, but it is not easy to see on ultrasound at that time.
CDH is a rare condition, affecting only 1 in every 2500 babies.
Depending on its size and position the hole in the diaphragm may allow any combination of stomach, bowel or part of the liver to move up from the abdomen into the chest. These take up space in the chest which means that the lung growth and development will be restricted. This can impact the wellbeing of the baby following birth and in some cases, will affect his or her ability to breath. This is a serious problem and will require your baby to be stabilised on a ventilator (a machine that supports breathing) before an operation to close the hole can take place, usually a few days following your baby’s birth.
There is no known single cause of CDH. It is not related to anything that the mother did or did not do during the pregnancy. Sometimes CDH is found with other problems such as a chromosomal or syndromic problem. Your doctor will talk to you about this in more detail.
How is a diaphragmatic hernia diagnosed?
CDH is often diagnosed during pregnancy at the point of the routine anatomy scan at 18 to 20 weeks. If a problem is suspected then you will be referred to the Fetal Medicine Department for a specialist scan and opinion to confirm the diagnosis.
Some cases of CDH are diagnosed following birth, when a baby shows signs of breathing difficulties.
What to expect during your pregnancy
Throughout your pregnancy you will be asked to attend frequent ultrasound scans and clinic appointments in the Fetal Medicine Department.
The purpose of these appointments is to:
- Identify whether there are any additional problems on ultrasound.
- A Magnetic Resonance Imaging (MRI) scan is offered to help assess the severity of the CDH and support the ultrasound findings.
- Offer of an amniocentesis to determine if the cause is due to a chromosome problem.
- Check for complications caused by the CDH such as polyhydramnios (too much amniotic fluid) which can lead to early labour.
- Introduce you to team members who will be involved with the care of the baby following birth including doctors from the neonatal and paediatric surgical teams.
The safest place for the baby to be delivered if you live in the North East or Cumbria is at the RVI, Newcastle upon Tyne, where specialist neonatal and paediatric surgical teams are based. During the course of your pregnancy, the fetal medicine team will organise transfer of your care for delivery from your local hospital to the RVI. Delivery, often by induction of labour, is usually arranged around 38-39 week’s gestation to ensure your baby arrives on a planned date and at the RVI. This will ensure all the medical teams involved are present at the birth and that there is an available cot in Neonatal Intensive Care Unit (NICU). Occasionally the planned date is changed due to other emergencies in the department meaning cots or incubators become unavailable for a short time.
If you go into labour sooner than expected you should attend your closest hospital for assessment.
All of your usual pregnancy care should still take place and it is important to still arrange to see your community midwife for routine antenatal appointments.
We recommend aiming for a vaginal delivery if possible. During a vaginal delivery the chest is normally compressed which allows fluid to come up from the lungs and out of the mouth. This helps with the first breaths.
What happens after your baby is born?
As soon as your baby is born, you can expect a lot of activity in the delivery room. Neonatal doctors and nurses will be present at the delivery and will need to review and intubate the baby immediately. This involves passing a small flexible tube into the baby’s trachea (airway) via their mouth. For feeding, a small tube (nasogastric tube) will also be inserted into your baby’s nose down to the stomach. Medication will be given to keep your baby still and comfortable.
To help with breathing a ventilator machine is attached to the breathing tube to assist and control your baby’s breathing.
Because of this it will not be possible to hold your baby immediately after birth but once they are stable the neonatal doctors will bring the baby close to you before they take the baby to the neonatal unit. After the baby is taken to the neonatal unit, they will undergo a series of investigations such as an x-ray and blood tests. You will be told about their progress and your midwife will check with the neonatal team to find out when it is possible for you to go to the neonatal unit to see your baby.
All types of diaphragmatic hernia are repaired by an operation under general anaesthetic. The paediatric surgeons will only perform the operation once your baby’s breathing is stable. This usually takes place a few days after the baby is born. He or she will be transferred in an incubator to theatre then to the Paediatric intensive care unit (PICU) for recovery.
Unfortunately, despite the expert input from the neonatal team, the breathing for some babies will never be stable enough to undergo a successful operation to repair the Congenital Diaphragmatic Hernia. These babies cannot survive for more than a few days following birth but the neonatal team will provide care to keep them comfortable until they die. The doctors in the neonatal unit will keep you regularly updated about the baby’s progress. It is impossible to accurately predict which babies will not survive following birth, but a rough estimation of surviving babies is in the region of 50%. For this reason, some women and couples feel that this correct choice for them is to consider a termination of pregnancy following the diagnosis. Your doctor will discuss this with you in more detail.
Can I stay with my baby?
Crawford House is situated within the grounds of the RVI and provides a “Home from Home” supporting families with children being treated at the RVI. Accommodation is provided for those who live outside of Newcastle and is provided free of charge by the registered charity, The Sick Children’s Trust. The house is available 365 days a year and has 23 private family bedrooms. There is a fully- equipped kitchen, dining area, playroom and living room alongside bathrooms and laundry facilities. Rooms are allocated on a priority basis and unfortunately cannot be pre booked before delivery. Once you are discharged from the Maternity Unit, accommodation can be booked.
For further information
For further information please contact:
Fetal Medicine Department,
Royal Victoria Infirmary
(0191) 2825837
Monday –Friday 9-5pm
Be sure to ask questions to the doctor supplying you with this leaflet and make a note of any questions you would like to ask at your next Fetal Medicine Unit appointment.
Antenatal Results and Choices
0845 077 2290 or 0207 713 7486 via mobile
North of Tyne Patient Advice and Liaison Service (PALS)
0800 0320202
Monday to Friday 9.00-4.30pm (answer phone out of hours)
Email: [email protected]
Resource Information
Information produced by Lesley Walker (Fetal Medicine Clinical Lead)
Date July 2019
Updated by Angela Lightfoot: 21/07/2023
Review date: July 2026