Surgeons at Newcastle Hospitals have performed the first robotic-assisted Total hip replacements in the North of England outside of a clinical trial.
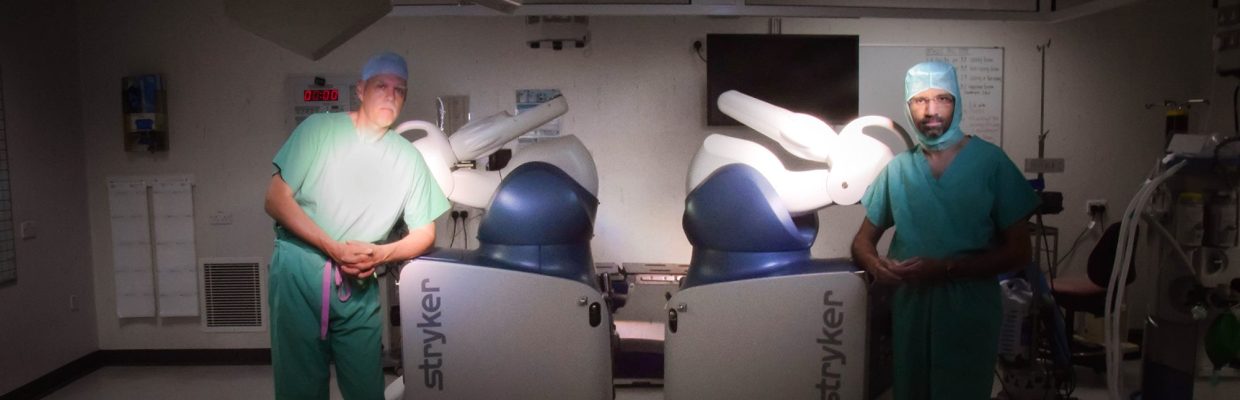
The orthopaedic team carried out the procedure on two patients in the Freeman Hospital last month using the Mako robot – visionary technology controlled by a highly skilled and experienced surgeon to help increase accuracy and precision.
Consultant orthopaedic surgeons, Prof. David Deehan and Mr. David Weir have been performing Mako Robotic knee replacements since 2019 as part of a major national study – known as the RACER-knee study – which is comparing traditional methods of knee replacement versus a surgeon using a robotic arm to carry out the procedure.
But it is thought to be the first time this cutting-edge technology has been used in the North of England for a hip replacement on an NHS patient outside of a clinical trial.
Compared to traditional surgery, benefits of robot-assisted surgery include:
- Reduced pain after surgery
- Less risk of damage to surrounding structures
- Allowing a faster recovery in total knee movement
- Performing joint replacement surgery with 2–3 times the accuracy.

Unlike traditional hip surgery, surgeons use a Mako to assist with the preparation and implant placement for joint replacement. The Mako uses a CT scan of the pelvis and femur, which is used to plan the placement of the implant, on a 3D model of the patient’s exact anatomy.
The robotic arm is then directed by the surgeon to help place the hip implant at the desired angle and inclination that will give the best bone coverage, stability and leg length for the patient. Mako gives the surgeon the auditory, visual, and tactile cues to help guide them in the right direction.
Consultant orthopaedic surgeon, Mr Sharad Bhatnagar who performed the first procedure, explains: “We have been using the Mako to perform knee replacements as part of a clinical trial for over two years. However, we believe these are the first two patients in the NHS to have this robotic assisted hip surgery outside of a clinical trial in the North of England.”
“All the planning is done before the operation with the help of Mako Product Specialist (MPS) on a computer software to plan implant placement. It also identifies the correct size implants to match patient’s anatomy.
“This has a potential advantage of decreasing the inventory and equipment needed for each patient. The planning software shows a virtual hip replacement in 3D which can be altered to allow optimum bone coverage and alignment. The fascinating thing is that the post-operative x-ray looks exactly like to image predicted by the robot.”
The robotic arm allows the surgeon to place the implants with high level of precision thereby reducing the chances of human error. This helps in accurately restoring patient’s centre of rotation of the hip and achieving planned limb lengthening.
As part of the operation, pin markers are inserted in the pelvis to help Mako match patient’s anatomy with the CT scan. After exposing the hip, the robotic arm comes in to prepare the acetabulum and implant the shell.
A complication of hip replacement is dislocation, which can occur in 1-2% of patients in the first six months after surgery. Due to the increased accuracy afforded by the Mako, the chance of dislocation and other complication should be reduced, improving patient outcomes.
This technology has been used to carry out complex hip replacements, one of these patients is 39-year-old Rosa Pires from Westerhope, who required a replacement following sickle cell crisis.
During a sickle cell crisis, pain develops when sickle-shaped red blood cells block blood flow through tiny blood vessels to the joints.
Sickle cell crisis manifested as end stage arthritis, causing extreme pain and deterioration of the left hip, after previous injury caused further complications, as Rosa explains:
“At 5-years-old, I was involved in an accident where I grew up in Mongolia, which left an open fracture in the right tibia caused my right leg to be shorter than my left,” she said.
“As time has gone on, this has caused me to put all my weight on my left leg.
I started to develop arthritis in my left hip. Despite pain killers, I was in constant pain struggling with activities of daily living.”
Rosa was due to have a hip replacement 4-years-ago, but as she was ready for surgery became pregnant with her third child, and soon after that, with her fourth.
Carrying a baby caused added strain on the joint, and 8-months after the birth of her fourth child, Rosa was in extreme pain and immobile:
“My hip was extremely painful. I could not walk from the kitchen to the living room without being in pain. I am young and am used to being independent, but I have had to rely on my husband doing everything for me,” Rosa adds.
Last month, Rosa had surgery to replace her hip, where it was explained to her that she would be one of the first to have a replacement with this new technique, Rosa comments:
“At first, I was a little worried about going for the procedure, but Mr Bhatnagar explained how the precision of the surgery would result in a more accurate result and reduced the chance of creating a bigger difference in length between my legs.”
Before surgery, Rosa underwent a blood transfusion to reduce the possibility of blood vessels becoming blocked causing further damage and to help reduce complications.
“All I wanted was to get my independence back, and with the robotic surgery I knew the recovery would be shorter and with my sickle cell disease it is important to reduce the chance of complications,” Rosa explained.
A few days later following monitoring for sickle cell disease crisis, Rosa was home following surgery to replace her hip. She has been walking with crutches and has already managed to catch a bus – enjoying getting her independence back.